Methods for Testing Pathogens
How to Test for Pathogens
Most bacteria are not harmful to human beings and exist as a normal flora. However if the microbe is harmful to humans and causes a disease then it is classed a pathogen. Since most test for pathogen in food is on bacteria, we describe tests only in this area.
To test for pathogen, you will have first decide on which pathogen to test for. To do this you can refer to your HACCP plan as this evaluates the risks for including or ignoring testing the selected pathogen. If your plan does not include pathogen testing you can get an audit from an external investigator familiar with pathogen control. Pathogen testing usually involves three areas, i.e. product, environmental, and equipment swabbing. The result of this testing is to ensure that the food you produce is safe for consumption and free of pathogen. Since pathogens can come from your raw materials and from your manufacturing environment (including production personnel) and can grow on your equipment from a previous infection, all three areas of testing are important and cannot be avoided. However since the implementation of the Food Safety Modernization Act, the emphasis on testing has been in the monitoring of the environment for indicator organism and for pathogens in the environment and less on the incoming raw materials. This is because most food production has a kill step for pathogens, resulting an emphasis for post contamination. Of course this is on the premise that environmental monitoring has been extended to the supplier. The selection of which pathogens to test is based on the history of the food product and its known pathogens. This is different from analysis of the final product which is quality control and which will result in a statistically safe risk of infection. Bioscience Diagnostics provides various platform for the detection of pathogens and its choice will depend time to result, cost, and accuracy required.
Methods for Testing Pathogens
There are various platforms for testing pathogens: -
- Conventional method with culture media,
- Immunoassay on ELISA microtiter plate,
- Immunoassay on Lateral Flow Sheets
- Enzyme technology on SimPlate,
- Enzyme technology for 100ml sample in bottle or Quanti-Tray,
- PCR technology.
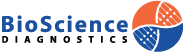
All methods include an enrichment step, followed by detection. Some tests require a confirmation step with a different method like culture media, PCR, or biochemical tests.
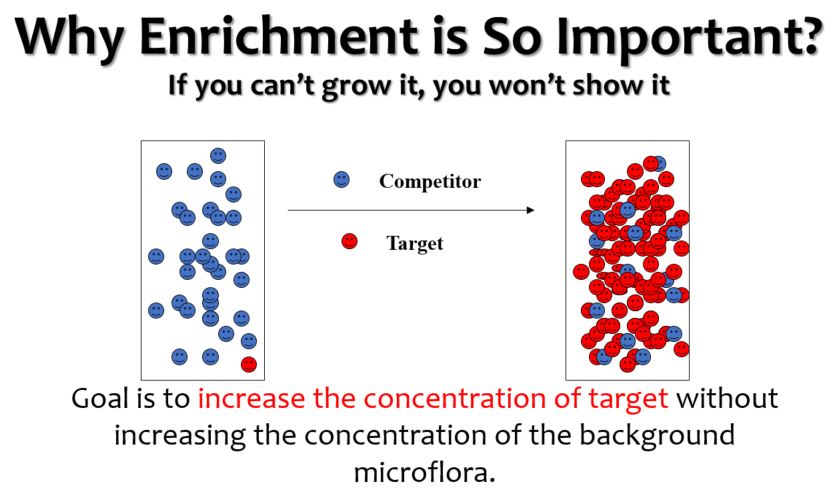
Specific Detection
Specific detection for rapid methods rely on antigens provided by the bacteria in the form of epitopes. These may be located on the cell body or on their flagella. The PCR method of detection looks at the representative conserve regions of the DNA for the particular pathogen.
Conventional Method for Pathogen Detection
There are generally two types of agar for detection of pathogens. One is nutrient agar with selective agents like antibiotics and the other uses a chromogenic compound to show a color differentiation.

BIOLIFE SS Agar is a selective and differential medium for the isolation and detection of salmonella with a direct inoculation after enrichment in a liquid media. The sodium citrate, bile salts and brilliant green inhibit the growth of gram positive bacteria and some non-pathogenic enteric bacteria. Lactose is the fermentable carbohydrate to differentiate the non-lactose fermenting bacteria from lactose fermenting ones. Neutral red is the pH indicator. When the medium becomes acid due to the fermentation of lactose, the bile salts precipitate and the medium takes on the color of the indicator. Sodium thiosulphate is added as the hydrogen sulfide source and ferric citrate is the indicator for hydrogen sulfide. Some species of proteus and salmonella produce black center due to the precipitation of iron sulphide. This agar is highly selective and strains of shigella will not grow.
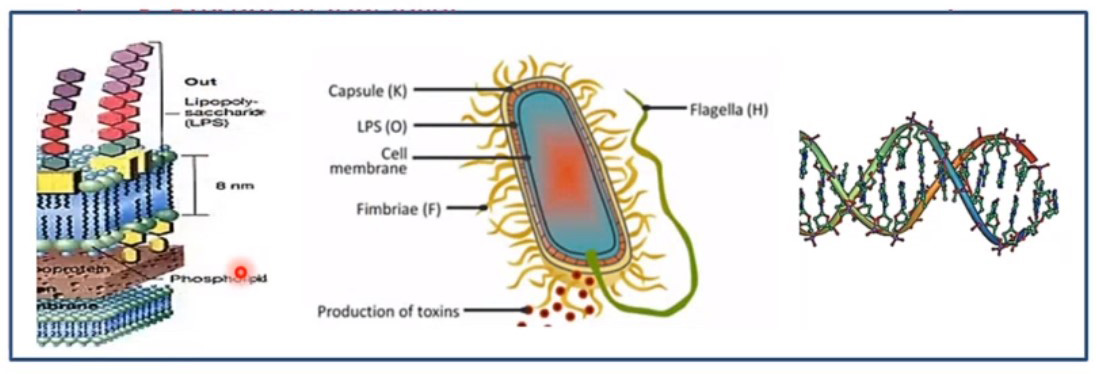
The common method for isolation of bacillus cereus recommended by ISO includes growth on MYP medium. Problems with MYP include a lack of characteristic colony morphology and they are often masked by background flora of other bacillus species. The above BIOLIFE medium includes a specific chromogen for the detection of the enzyme β-glucosidase and a substrate for the detection of phospholipase. Colonies of B cereus and their group are blue green with a typical zone of precipitation (except B anthracis). The antibiotic mix strongly reduces the background of gram negative and gram positive bacteria and allow the isolation of the B. Cereus group often in pure culture.

ELISA detection of pathogens depend on the antibody and antigen binding. The antibody (shaped Y) is bound onto the base of a microtiter plate. Any antigen i.e. bacteria specific to the antibody will attach itself to it. Then an antibody enzyme conjugate is added which will bind specifically to the antigen or pathogen. A substrate is finally added to give a colored complex the strength of which will quantify the amount of bacteria present.

We provide the best services about science.
About Company
Sitemap
Please contact our friendly sales staff for more information.
Feel free to ask us questions. We would love to assist you !